Twinrix: Package Insert / Prescribing Info
Package insert / product label
Generic name: hepatitis a and hepatitis b (recombinant) vaccine
Dosage form: injection, suspension
Drug class: Vaccine combinations
Medically reviewed by Drugs.com. Last updated on Jul 16, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- References
- How Supplied/Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
TWINRIX [Hepatitis A & Hepatitis B (Recombinant) Vaccine] injectable suspension, for intramuscular use
Initial U.S. Approval: 2001
Indications and Usage for Twinrix
TWINRIX is a vaccine indicated for active immunization against disease caused by hepatitis A virus and infection by all known subtypes of hepatitis B virus. TWINRIX is approved for use in persons 18 years of age or older. (1)
Twinrix Dosage and Administration
Dosage Forms and Strengths
Contraindications
Severe allergic reaction (e.g., anaphylaxis) after a previous dose of any hepatitis A-containing or hepatitis B-containing vaccine, or to any component of TWINRIX, including yeast and neomycin. (4)
Warnings and Precautions
- Syncope (fainting) can occur in association with administration of injectable vaccines, including TWINRIX. Procedures should be in place to avoid falling injury and to restore cerebral perfusion following syncope. (5.1)
Adverse Reactions/Side Effects
Following any dose of TWINRIX, the most common (≥10%) solicited injection site reactions were injection site soreness (35% to 41%) and redness (8% to 11%); the most common solicited systemic adverse reactions were headache (13% to 22%) and fatigue (11% to 14%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.
Drug Interactions
Do not mix TWINRIX with any other vaccine or product in the same syringe. (7.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2024
Full Prescribing Information
1. Indications and Usage for Twinrix
TWINRIX is indicated for active immunization against disease caused by hepatitis A virus and infection by all known subtypes of hepatitis B virus. TWINRIX is approved for use in persons 18 years of age or older.
2. Twinrix Dosage and Administration
2.1 Preparation for Administration
The vaccine should be re-suspended before use. When re-suspended, the vaccine will have a uniform hazy white appearance.
Upon storage, a fine white deposit with a clear colorless layer above may be present. Re-suspend the vaccine following the steps below.
1. Hold the syringe upright in a closed hand.
2. Shake the syringe by tipping it upside down and back upright again.
3. Repeat this action vigorously for at least 15 seconds.
4. Inspect the vaccine again:
- •
- If the vaccine appears as a uniform hazy white suspension, it is ready to use – the appearance should not be clear.
- •
- If the vaccine still does not appear as a uniform hazy white suspension, tip upside down and back upright again for at least another 15 seconds then inspect again.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If either of these conditions exists, the vaccine should not be administered.
Attach a sterile needle to the prefilled syringe and administer intramuscularly.
2.2 Administration
TWINRIX should be administered by intramuscular injection only as a 1-mL dose. Administer in the deltoid region. Do not administer in the gluteal region; such injections may result in a suboptimal response.
Do not administer this product intravenously, intradermally, or subcutaneously.
2.3 Recommended Dose and Schedule
Standard dosing schedule consists of 3 doses (1-mL each), given intramuscularly at 0, 1, and 6 months. Alternatively, an accelerated schedule of 4 doses (1-mL each), given intramuscularly on Days 0, 7, and 21 to 30 followed by a booster dose at Month 12 may be used.
3. Dosage Forms and Strengths
Suspension for injection available in 1-mL prefilled TIP-LOK syringes [see Description (11), How Supplied/Storage and Handling (16)].
4. Contraindications
Severe allergic reaction (e.g., anaphylaxis) after a previous dose of any hepatitis A-containing or hepatitis B-containing vaccine, or to any component of TWINRIX, including yeast and neomycin, is a contraindication to administration of TWINRIX [see Description (11)].
5. Warnings and Precautions
5.1 Syncope
Syncope (fainting) can occur in association with administration of injectable vaccines, including TWINRIX. Syncope can be accompanied by transient neurological signs such as visual disturbance, paresthesia, and tonic-clonic limb movements. Procedures should be in place to avoid falling injury and to restore cerebral perfusion following syncope.
5.2 Preventing and Managing Allergic Vaccine Reactions
Prior to immunization, the healthcare provider should review the immunization history for possible vaccine sensitivity and previous vaccination-related adverse reactions to allow an assessment of benefits and risks. Appropriate medical treatment and supervision must be available to manage possible anaphylactic reactions following administration of the vaccine. [See Contraindications (4).]
5.3 Moderate or Severe Acute Illness
To avoid diagnostic confusion between manifestations of an acute illness and possible vaccine adverse effects, vaccination with TWINRIX should be postponed in persons with moderate or severe acute febrile illness unless they are at immediate risk of hepatitis A or hepatitis B infection.
5.4 Altered Immunocompetence
Immunocompromised persons, including individuals receiving immunosuppressive therapy, may have a diminished immune response to TWINRIX.
5.5 Multiple Sclerosis
Results from 2 clinical studies indicate that there is no association between hepatitis B vaccination and the development of multiple sclerosis,1 and that vaccination with hepatitis B vaccine does not appear to increase the short-term risk of relapse in multiple sclerosis.2
5.6 Limitations of Vaccine Effectiveness
Hepatitis A and hepatitis B have relatively long incubation periods. The vaccine may not prevent hepatitis A or hepatitis B infection in individuals who have an unrecognized hepatitis A or hepatitis B infection at the time of vaccination. Additionally, vaccination with TWINRIX may not protect all individuals.
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Following any dose of TWINRIX, the most common (≥10%) solicited injection site reactions were injection site soreness (35% to 41%) and redness (8% to 11%); the most common solicited systemic adverse reactions were headache (13% to 22%) and fatigue (11% to 14%).
The safety of TWINRIX has been evaluated in clinical trials involving the administration of approximately 7,500 doses to more than 2,500 individuals.
In a U.S. study, 773 subjects (aged 18 to 70 years) were randomized 1:1 to receive TWINRIX (0-, 1-, and 6-month schedule) or concurrent administration of ENGERIX-B (0-, 1-, and 6-month schedule) and HAVRIX (0- and 6-month schedule). Solicited local adverse reactions and systemic adverse events were recorded by parents/guardians on diary cards for 4 days (Days 0 to 3) after vaccination. Unsolicited adverse events were recorded for 31 days after vaccination. Solicited reactions reported following the administration of TWINRIX or ENGERIX-B and HAVRIX are presented in Table 1.
|
Local |
TWINRIX |
ENGERIX-B |
HAVRIX |
|||||
|
Dose 1 |
Dose 2 |
Dose 3 |
Dose 1 |
Dose 2 |
Dose 3 |
Dose 1 |
Dose 2 |
|
|
(n = 385) % |
(n = 382) % |
(n = 374) % |
(n = 382) % |
(n = 376) % |
(n = 369) % |
(n = 382) % |
(n = 369) % |
|
|
Soreness |
37 |
35 |
41 |
41 |
25 |
30 |
53 |
47 |
|
Redness |
8 |
9 |
11 |
6 |
7 |
9 |
7 |
9 |
|
Swelling |
4 |
4 |
6 |
3 |
5 |
5 |
5 |
5 |
|
Systemic |
TWINRIX |
ENGERIX-B and HAVRIX |
||||||
|
Dose 1 |
Dose 2 |
Dose 3 |
Dose 1d |
Dose 2e |
Dose 3d |
|||
|
(n = 385) % |
(n = 382) % |
(n = 374) % |
(n = 382) % |
(n = 376) % |
(n = 369) % |
|||
|
Headache |
22 |
15 |
13 |
19 |
12 |
14 |
||
|
Fatigue |
14 |
13 |
11 |
14 |
9 |
10 |
||
|
Diarrhea |
5 |
4 |
6 |
5 |
3 |
3 |
||
|
Nausea |
4 |
3 |
2 |
7 |
3 |
5 |
||
|
Fever |
4 |
3 |
2 |
4 |
2 |
4 |
||
|
Vomiting |
1 |
1 |
0 |
1 |
1 |
1 |
||
- a Within 4 days of vaccination defined as day of vaccination and the next 3 days.
- b 389 subjects received at least 1 dose of TWINRIX.
- c 384 subjects received at least 1 dose each of ENGERIX-B and HAVRIX.
- d Doses 1 and 3 included ENGERIX-B and HAVRIX in the control group receiving separate vaccinations.
- e Dose 2 included only ENGERIX-B in the control group receiving separate vaccinations.
Most solicited local adverse reactions and systemic adverse reactions seen with TWINRIX were considered by the subjects as mild and self-limiting and did not last more than 48 hours.
In a clinical trial in which TWINRIX was given on a 0-, 7-, and 21- to 30-day schedule followed by a booster dose at 12 months, solicited local adverse reactions or systemic adverse reactions were comparable to those seen in other clinical trials of TWINRIX given on a 0-, 1-, and 6-month schedule.
Among 2,299 subjects in 14 clinical trials, the following adverse reactions were reported to occur within 30 days following vaccination:
Incidence 1% to 10% of Injections, Seen in Clinical Trials with TWINRIX
Infections and Infestations: Upper respiratory tract infections.
General Disorders and Administration Site Conditions: Injection site induration.
Incidence <1% of Injections, Seen in Clinical Trials with TWINRIX
Infections and Infestations: Respiratory tract illnesses.
Metabolism and Nutrition Disorders: Anorexia.
Psychiatric Disorders: Agitation, insomnia.
Nervous System Disorders: Dizziness, migraine, paresthesia, somnolence, syncope.
Ear and Labyrinth Disorders: Vertigo.
Vascular Disorders: Flushing.
Gastrointestinal Disorders: Abdominal pain, vomiting.
Skin and Subcutaneous Tissue Disorders: Erythema, petechiae, rash, sweating, urticaria.
Musculoskeletal and Connective Tissue Disorders: Arthralgia, back pain, myalgia.
General Disorders and Administration Site Conditions: Injection site ecchymosis, injection site pruritus, influenza-like symptoms, irritability, weakness.
Incidence <1% of Injections, Seen in Clinical Trials with HAVRIX and/or ENGERIX-B
Blood and Lymphatic System Disorders: Lymphadenopathy.a+b
Nervous System Disorders: Dysgeusia,a hypertonia,a tingling.b
Eye Disorders: Photophobia.a
Vascular Disorders: Hypotension.b
Gastrointestinal Disorders: Constipation.b
Investigations: Creatine phosphokinase increased.a
- a+b Following either HAVRIX or ENGERIX B.
- a Following HAVRIX.
- b Following ENGERIX B.
Adverse reactions within 30 days of vaccination in the U.S. clinical trial of TWINRIX given on a 0-, 7-, and 21- to 30-day schedule followed by a booster dose at 12 months were comparable to those reported in other clinical trials.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of TWINRIX, HAVRIX, or ENGERIX-B. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to the vaccine.
Postmarketing Experience with TWINRIX
Infections and Infestations: Herpes zoster, meningitis.
Blood and Lymphatic System Disorders: Thrombocytopenia, thrombocytopenic purpura.
Immune System Disorders: Allergic reaction, anaphylactoid reaction, anaphylaxis, serum sickness–like syndrome days to weeks after vaccination (including arthralgia/arthritis, usually transient; fever; urticaria; erythema multiforme; ecchymoses; and erythema nodosum).
Nervous System Disorders: Bell's palsy, convulsions, encephalitis, encephalopathy, Guillain-Barré syndrome, hypoesthesia, myelitis, multiple sclerosis, neuritis, neuropathy, optic neuritis, paralysis, paresis, transverse myelitis.
Eye Disorders: Conjunctivitis, visual disturbances.
Ear and Labyrinth Disorders: Earache, tinnitus.
Cardiac Disorders: Palpitations, tachycardia.
Vascular Disorders: Vasculitis.
Respiratory, Thoracic, and Mediastinal Disorders: Bronchospasm, including asthma-like symptoms; dyspnea.
Gastrointestinal Disorders: Dyspepsia.
Hepatobiliary Disorders: Hepatitis, jaundice.
Skin and Subcutaneous Tissue Disorders: Alopecia, angioedema, eczema, erythema multiforme, erythema nodosum, hyperhidrosis, lichen planus.
Musculoskeletal and Connective Tissue Disorders: Arthritis, muscular weakness.
General Disorders and Administration Site Conditions: Chills; immediate injection site pain, stinging, and burning sensation; injection site reaction; malaise.
Investigations: Abnormal liver function tests.
Postmarketing Experience with HAVRIX and/or ENGERIX-B
The following list includes adverse reactions for HAVRIX and/or ENGERIX-B not already reported above for TWINRIX.
Eye Disorders: Keratitis.a
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome.a
Congenital, Familial, and Genetic Disorders: Congenital abnormality.b
- a Following ENGERIX-B.
- b Following HAVRIX.
7. Drug Interactions
7.1 Concomitant Administration with Vaccines and Immune Globulin
Do not mix TWINRIX with any other vaccine or product in the same syringe.
When concomitant administration of immunoglobulin is required, it should be given with a different syringe and at a different injection site.
There are no data to assess the concomitant use of TWINRIX with other vaccines.
7.2 Immunosuppressive Therapies
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs, and corticosteroids (used in greater-than-physiologic doses), may reduce the immune response to TWINRIX.
7.3 Interference with Laboratory Tests
Hepatitis B surface antigen (HBsAg) derived from hepatitis B vaccines has been transiently detected in blood samples following vaccination. Serum HBsAg detection may not have diagnostic value within 28 days after receipt of a hepatitis B vaccine, including TWINRIX.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
There are no adequate and well-controlled studies of TWINRIX in pregnant women in the U.S. Available data do not suggest an increased risk of major birth defects and miscarriage in women who received TWINRIX within 28 days prior to conception or during pregnancy (see Data).
A developmental toxicity study was performed in female rats administered TWINRIX prior to mating and during gestation (0.2 mL at each occasion). This study revealed no adverse effects on fetal or pre-weaning development (see Data).
Data
Human Data: A pregnancy exposure registry was maintained from 2001 to 2015. The registry prospectively enrolled 245 women who received a dose of TWINRIX during pregnancy or within 28 days prior to conception. After excluding induced abortions (n = 6, including one of a fetus with congenital anomalies), those lost to follow-up (n = 142), those with exposure in the third trimester (n = 1), and those with an unknown exposure timing (n = 9), there were 87 pregnancies with known outcomes with exposure within 28 days prior to conception, or in the first or second trimesters. Miscarriage was reported for 9.6% of pregnancies with exposure to TWINRIX prior to 20 weeks gestation (8/83). Major birth defects were reported for 3.8% of live born infants whose mothers were exposed within 28 days prior to conception or during the first or second trimester (3/80). The rates of miscarriage and major birth defects were consistent with estimated background rates.
In pre- and post-licensure clinical studies of TWINRIX, 45 pregnant women were inadvertently administered TWINRIX following their last menstrual period. Among such pregnancies, after excluding elective terminations (n = 1) and those lost to follow-up (n = 1), there were 43 pregnancies with known outcomes all with exposure in the first trimester. Miscarriage was reported in 16% of pregnancies (7/43) and major birth defects were reported in 2.6% of live births (1/38). The rates of miscarriage and major birth defects were consistent with estimated background rates.
Animal Data: In a developmental toxicity study, female rats were administered TWINRIX by intramuscular injection on Day 30 prior to mating and on gestation Days 6, 8, 11, and 15. The total dose was 0.2 mL (divided) at each occasion (a single human dose is 1 mL). No adverse effects on pre-weaning development up to post-natal Day 25 were observed. There were no fetal malformations or variations.
8.2 Lactation
Risk Summary
There is no information regarding the presence of TWINRIX in human milk, the effects on the breastfed child, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for TWINRIX and any potential adverse effects on the breastfed child from TWINRIX or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
11. Twinrix Description
TWINRIX [Hepatitis A & Hepatitis B (Recombinant) Vaccine] is a bivalent vaccine containing the antigenic components used in producing HAVRIX (Hepatitis A Vaccine) and ENGERIX-B [Hepatitis B Vaccine (Recombinant)]. TWINRIX is a sterile suspension for intramuscular administration that contains inactivated hepatitis A virus (strain HM175) and noninfectious HBsAg. The hepatitis A virus is propagated in MRC-5 human diploid cells and inactivated with formalin. The purified HBsAg is obtained by culturing genetically engineered Saccharomyces cerevisiae yeast cells, which carry the surface antigen gene of the hepatitis B virus. Bulk preparations of each antigen are adsorbed separately onto aluminum salts and then pooled during formulation.
A 1-mL dose of vaccine contains 720 ELISA Units of inactivated hepatitis A virus and 20 mcg of recombinant HBsAg protein. One dose of vaccine also contains 0.45 mg of aluminum in the form of aluminum phosphate and aluminum hydroxide as adjuvants, amino acids, sodium chloride, phosphate buffer, polysorbate 20, and Water for Injection. From the manufacturing process, each 1-mL dose of TWINRIX also contains residual formalin (not more than 0.1 mg), MRC-5 cellular proteins (not more than 2.5 mcg), neomycin sulfate (an aminoglycoside antibiotic included in the cell growth media; not more than 20 ng), and yeast protein (no more than 5%).
TWINRIX is available in prefilled syringes. The tip cap and rubber plunger stopper of the prefilled syringe are not made with natural rubber latex.
TWINRIX is formulated without preservatives.
12. Twinrix - Clinical Pharmacology
12.1 Mechanism of Action
Hepatitis A
The course of infection with hepatitis A virus (HAV) is extremely variable, ranging from asymptomatic infection to fulminant hepatitis.3
The presence of antibodies to HAV (anti-HAV) confers protection against hepatitis A disease. However, the lowest titer needed to confer protection has not been determined. Natural infection provides lifelong immunity even when antibodies to hepatitis A are undetectable. Seroconversion is defined as antibody titers equal to or greater than the assay cut-off (cut-off values vary depending on the assay used) in those previously seronegative.
Hepatitis B
Infection with hepatitis B virus (HBV) can have serious consequences including acute massive hepatic necrosis and chronic active hepatitis. Chronically infected persons are at increased risk for cirrhosis and hepatocellular carcinoma.
Antibody concentrations ≥10 mIU/mL against HBsAg are recognized as conferring protection against hepatitis B virus infection.4
14. Clinical Studies
14.1 Immunogenicity: Standard 0-, 1-, and 6-Month Dosing Schedule
In 11 clinical trials, sera from 1,551 healthy adults aged 17 to 70 years, including 555 male subjects and 996 female subjects, were analyzed following administration of 3 doses of TWINRIX on a 0-, 1-, and 6-month schedule. Seroconversion (defined as equal to or greater than assay cut-off depending on assay used) for antibodies against HAV was elicited in 99.9% of vaccinees, and protective antibodies (defined as ≥10 mIU/mL) against HBV surface antigen were detected in 98.5% of vaccinees, 1 month after completion of the 3-dose series (Table 2).
|
Dose of TWINRIX |
n |
% Seroconversion for Hepatitis Aa |
% Seroprotection for Hepatitis Bb |
|
1 |
1,587 |
93.8 |
30.8 |
|
2 |
1,571 |
98.8 |
78.2 |
|
3 |
1,551 |
99.9 |
98.5 |
- a Anti‑HAV titer ≥assay cut‑off: 20 mIU/mL (HAVAB Test) or 33 mIU/mL (ENZYMUN‑TEST).
- b Anti‑HBsAg titer ≥10 mIU/mL (AUSAB Test).
One of the 11 trials was a comparative trial conducted in a U.S. population given either TWINRIX (on a 0-, 1-, and 6-month schedule) or HAVRIX (0- and 6-month schedule) and ENGERIX-B (0-, 1-, and 6-month schedule). The monovalent vaccines were given concurrently in opposite arms. Of the 773 adults (aged 18 to 70 years) enrolled in this trial, an immunogenicity analysis was performed in 533 subjects who completed the study according to protocol. Of these, 264 subjects received TWINRIX and 269 subjects received HAVRIX and ENGERIX-B. Seroconversion rates against HAV and seroprotection rates against HBV are presented in Table 3; geometric mean titers (GMTs) are presented in Table 4. The absolute difference in anti-HAV seropositivity rates between groups was 0.36% (90% CI: -1.8, 3.1). Non-inferiority in terms of anti-HAV response was demonstrated (lower limit of the 90% CI was higher than the pre-specified non-inferiority criterion of -4.3%). The absolute difference in anti-HBsAg seroprotection rates between groups was 2.8% (90% CI: -1.3, 7.7). Non-inferiority in terms of anti-HBV response was demonstrated (lower limit of the 90% CI was higher than the pre-specified non-inferiority criterion of -9.4%).
|
Vaccine |
n |
Timepoint |
% Seroconversion for Hepatitis Aa (95% CI) |
% Seroprotection for Hepatitis Bb (95% CI) |
|
TWINRIX |
264 |
Month 1 |
91.6 |
17.9 |
|
Month 2 |
97.7 |
61.2 |
||
|
Month 7 |
99.6 (97.9, 100.0) |
95.1 (91.7, 97.4) |
||
|
HAVRIX and ENGERIX-B |
269 |
Month 1 |
98.1 |
7.5 |
|
Month 2 |
98.9 |
50.4 |
||
|
Month 7 |
99.3 (97.3, 99.9) |
92.2 (88.3, 95.1) |
- CI = Confidence Interval.
- a Anti-HAV titer ≥assay cut-off: 33 mIU/mL (ENZYMUN-TEST).
- b Anti-HBsAg titer ≥10 mIU/mL (AUSAB Test).
|
Vaccine |
n |
Timepoint |
GMT to Hepatitis A (95% CI) |
GMT to Hepatitis B (95% CI) |
|
TWINRIX |
263 |
Month 1 |
335 |
8 |
|
259 |
Month 2 |
636 |
23 |
|
|
264 |
Month 7 |
4756 (4152, 5448) |
2099 (1663, 2649) |
|
|
HAVRIX and ENGERIX-B |
268 |
Month 1 |
444 |
6 |
|
269 |
Month 2 |
257 |
18 |
|
|
269 |
Month 7 |
2948 (2638, 3294) |
1871 (1428, 2450) |
- GMT = Geometric mean titer; CI = Confidence Interval.
Since the immune responses to hepatitis A and hepatitis B induced by TWINRIX were non-inferior to the monovalent vaccines, efficacy is expected to be similar to the efficacy for each of the monovalent vaccines.
The antibody titers achieved 1 month after the final dose of TWINRIX were higher than titers achieved 1 month after the final dose of HAVRIX in this clinical trial. This may have been due to a difference in the recommended dosage regimens for these 2 vaccines, whereby vaccinees receiving TWINRIX received 3 doses of 720 EL.U. of hepatitis A antigen at 0, 1, and 6 months, whereas vaccinees receiving HAVRIX received 2 doses of 1440 EL.U. of the same antigen (at 0 and 6 months). However, these differences in peak titer have not been shown to be clinically significant.
14.2 Immunogenicity: Accelerated Dosing Schedule (Day 0, 7, and 21 to 30, Month 12)
In 496 healthy adults, the safety and immunogenicity of TWINRIX given on a 0-, 7-, and 21- to 30-day schedule followed by a booster dose at 12 months (n = 250), was compared with separate vaccinations with monovalent hepatitis A vaccine (HAVRIX at 0 and 12 months) and hepatitis B vaccine (ENGERIX-B at 0, 1, 2, and 12 months) as a control group (n = 246).
Following a booster dose at Month 12, seroprotection rates for hepatitis B and seroconversion rates for hepatitis A at Month 13 following TWINRIX were non-inferior to the control group. The absolute difference in anti-HBs seroprotection rates between groups (HAVRIX + ENGERIX-B minus TWINRIX) was -2.99 (95% CI: -7.80, 1.49). Non-inferiority was demonstrated as the upper limit of the 95% CI was lower than the pre-defined limit of 7%. The absolute difference in anti-HAV seroprotection rates between groups (HAVRIX + ENGERIX-B minus TWINRIX) was 0 (95% CI: -1.91, 1.94). Non-inferiority was demonstrated as the upper limit of the 95% CI was lower than the pre-defined limit of 7%. The immune responses are presented in Table 5.
|
Timepoint |
TWINRIXa |
HAVRIX and ENGERIX-Bb |
|
|
(n = 194-204) |
(n = 197-207) |
||
|
% Seroconversion for Hepatitis Ac (95% CI) |
Day 37 |
98.5 (95.8, 99.7) |
98.6 (95.8, 99.7) |
|
Day 90 |
100 (98.2, 100) |
95.6 (91.9, 98.0) |
|
|
Month 12 |
96.9 (93.4, 98.9) |
86.9 (81.4, 91.2) |
|
|
Month 13 |
100 (98.1, 100) |
100 (98.1, 100) |
|
|
% Seroprotection for Hepatitis Bd (95% CI) |
Day 37 |
63.2 (56.2, 69.9) |
43.5 (36.6, 50.5) |
|
Day 90 |
83.2 (77.3, 88.1) |
76.7 (70.3, 82.3) |
|
|
Month 12 |
82.1 (75.9, 87.2) |
77.8 (71.3, 83.4) |
|
|
Month 13 |
96.4 (92.7, 98.5) |
93.4 (89.0, 96.4) |
- CI = Confidence Interval.
- a TWINRIX given on a 0-, 7-, and 21- to 30-day schedule followed by a booster at Month 12.
- b HAVRIX 1440 EL.U./1 mL given on a 0- and 12-month schedule and ENGERIX-B 20 mcg/1 mL given on a 0-, 1-, 2-, and 12-month schedule.
- c Anti-HAV titer ≥assay cut-off: 15 mIU/mL (anti-HAV Behring Test).
- d Anti‑HBsAg titer ≥10 mIU/mL (AUSAB Test).
14.3 Immunogenicity in Adults Older than 40 Years
The effect of age on immune response to TWINRIX was studied in 2 trials. The first trial evaluated subjects aged 41 to 63 years (N = 72; mean age = 50). All subjects were seropositive for anti-HAV antibodies following the third dose of TWINRIX. For the hepatitis B response, 94% of subjects were seroprotected after the third dose of TWINRIX.
The second trial included subjects aged 19 years and older with a comparison between those older than 40 years (n = 183, aged 41 to 70 years; mean age: 48) and those aged 40 years or younger (n = 191; aged 19 to 40 years; mean age: 33). More than 99% of subjects in both age groups achieved a seropositive response for anti-HAV antibodies, and GMTs were comparable between the age groups. In the older subjects who received TWINRIX, 92.9% (95% CI: 88.2, 96.2) achieved seroprotection against hepatitis B compared with 96.9% (95% CI: 93.3, 98.8) of the younger subjects. The GMT was 1,890 mIU/mL in the older subjects compared with 2,285 mIU/mL in the younger subjects.
14.4 Duration of Immunity
Two clinical trials involving a total of 129 subjects demonstrated that antibodies to both HAV and HBV surface antigen persisted for at least 4 years after the first vaccine dose in a 3-dose series of TWINRIX, given on a 0-, 1-, and 6-month schedule. For comparison, after the recommended immunization regimens for HAVRIX and ENGERIX-B, respectively, similar studies involving a total of 114 subjects have shown that seropositivity to HAV and HBV also persists for at least 4 years.
15. References
- 1.
- Ascherio A, Zhang SM, Hernán MA, et al. Hepatitis B vaccination and the risk of multiple sclerosis. N Engl J Med. 2001;344(5):327-332.
- 2.
- Confavreux C, Suissa S, Saddier P, et al. Vaccination and the risk of relapse in multiple sclerosis. N Engl J Med. 2001;344(5):319-326.
- 3.
- Lemon SM. Type A viral hepatitis: new developments in an old disease. N Engl J Med. 1985;313(17):1059-1067.
- 4.
- Frisch-Niggemeyer W, Ambrosch F, Hofmann H. The assessment of immunity against hepatitis B after vaccination. J Bio Stand. 1986;14(3):255-258.
16. How is Twinrix supplied
TWINRIX is available in 1-mL single-dose prefilled disposable TIP‑LOK syringes (Luer Lock syringes) packaged without needles (Preservative-Free Formulation). TIP-LOK syringes are to be used with Luer Lock compatible needles.
The tip cap and rubber plunger stopper of the prefilled syringe are not made with natural rubber latex.
NDC 58160-815-43 Syringe in Package of 10: NDC 58160-815-52
Store refrigerated between 2° and 8°C (36° and 46°F). Do not freeze; discard if product has been frozen.
17. Patient Counseling Information
- •
- Inform vaccine recipients of the potential benefits and risks of immunization with TWINRIX.
- •
- Emphasize, when educating vaccine recipients regarding potential side effects, that components of TWINRIX cannot cause hepatitis A or hepatitis B infection.
- •
- Instruct vaccine recipients to report any adverse events to their healthcare provider.
- •
- Give vaccine recipients the Vaccine Information Statements, which are required by the National Childhood Vaccine Injury Act of 1986 to be given prior to immunization. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
TWINRIX, HAVRIX, ENGERIX-B, and TIP-LOK are trademarks owned by or licensed to the GSK group of companies. The other brands listed are trademarks owned by or licensed to their respective owners and are not owned by or licensed to the GSK group of companies. The makers of these brands are not affiliated with and do not endorse the GSK group of companies or its products.
Manufactured by GlaxoSmithKline Biologicals
Rixensart, Belgium, U.S. License No. 1617
Distributed by GlaxoSmithKline
Durham, NC 27701
©2024 GSK group of companies or its licensor.
TWR:29PI
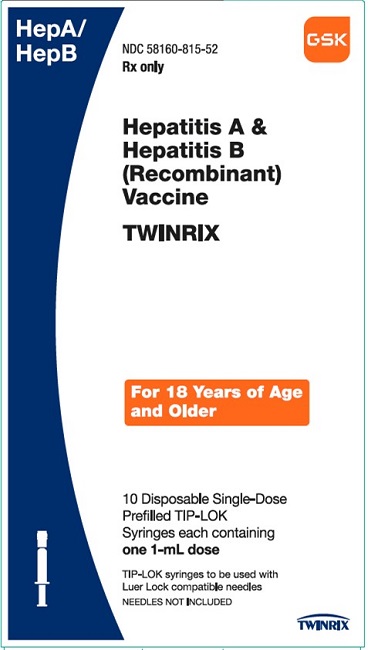
PRINCIPAL DISPLAY PANEL
NDC 58160-815-52
Hepatitis A & Hepatitis B (Recombinant) Vaccine
TWINRIX
HepA/HepB
Rx only
For 18 Years of Age and Older
10 Disposable Single-Dose Prefilled TIP-LOK Syringes each containing one 1-mL dose
TIP-LOK Syringes to be used with Luer Lock compatible needles
NEEDLES NOT INCLUDED
GSK
TWINRIX
Made in Belgium
©2023 GSK group of companies or its licensor.
Rev. 7/23
515698
| TWINRIX
hepatitis a and hepatitis b (recombinant) vaccine injection, suspension |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - GlaxoSmithKline Biologicals SA (372748392) |
More about Twinrix (hepatitis a adult vaccine / hepatitis b adult vaccine)
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: vaccine combinations
- En español